Author: Adam Bunker
Subject Matter Experts: Chelsea McKinney and Matt Lauer
Since the beginning of 2020, healthcare systems around the world have modernized at an incredible rate, with patient experience at the heart of the transformation.
In this guide, we’ll explore what patient experience is, how it can be improved, and how it’s helping healthcare organizations deliver more human-centered care.
What is patient experience?
When we’re defining patient experience, we’re really talking about how we can measure patients’ perceptions of the care they receive – at every touchpoint during their journey along the healthcare continuum.
The Beryl Institute suggests that patience experience measures:
The sum of all interactions, shaped by an organization’s culture, that influence a patient’s perspective along the continuum of care.
There are four critical components of that definition:
1. The sum of all interactions
A patient’s perspective about their medical care isn’t decided by a single service or visit, but rather is influenced by all the touchpoints along the patient journey, with each one playing a part in influencing their experience. Understanding how each process, touchpoint, and interaction can be optimized to improve the overall patient experience is essential.
2. An organization’s culture
The vision and values at every level of a healthcare organization play a vital role in the delivery of safe, convenient, and competent healthcare. From nurses and doctors directly caring for patients, to contact center agents and medical administrative staff, every healthcare employee has a role to play when it comes to patient experience.
3. How we can influence patient perceptions
This area of patient experience covers what is recognized, understood, and remembered by patients. It’s important to remember, there’s no one-size-fits-all — each individual’s perception of care from physicians and Advanced Practice Professionals (APPs) – and health systems – will be impacted by their own circumstances, beliefs, values, and cultural background.
4. The continuum of care
When measuring patient experience, many health systems only focus on what happens in healthcare facilities, like at a hospital or during a clinician visit. However, an individual’s experience with the healthcare system starts long before they begin to seek help, and continues long after they receive services – as part of a life-long journey to continued wellness.
World-class patient experience programs understand the role of a healthcare provider before, during, and after care delivery and respond to patients’ needs at every stage along that journey.
Free eBook: 2025 healthcare experience trends report
The evolution of patient satisfaction to patient experience
We’re often asked about the difference between patient satisfaction and patient experience, but patient satisfaction is a legacy concept – a measurement of a single interaction that uses a metric. And that’s more applicable to buying a product from Amazon, or streaming a film on Netflix.
Patient satisfaction ignores every activity outside of the specific interaction the patient was surveyed about – and it doesn’t truly link to patients’ expectations.
Let’s face it, nobody needs to be “satisfied” with their healthcare – they want safe, convenient, and competent care that leads to positive clinical outcomes. That’s the bar that healthcare organizations should set out to meet, and therefore measure how they’re performing against.

None of those are measured by asking, “How satisfied were you with your hospital visit today?”
Instead, taking a human-centered care approach, and considering the holistic experience patients have across their journey with a provider, offers much more actionable insights at every level of the organization.
That also includes analyzing the person-to-person interactions that help patients feel heard and understood, rather than as a number on a sheet or a diagnosis to fix. When acted upon in a unified way, all this information can help improve health outcomes, patient safety, and quality of care.
Listen to patients across the entire patient journey
All healthcare providers get patient feedback. After all, funding and reimbursements depend on it – so measurement is nothing new in the industry. But measurement is not the goal. You need to be asking these key questions:
- Are you listening on the right channels across the entire patient journey?
- Does every team and department in the organization understand how they impact the patient experience?
- And are those people empowered to take actions that will influence perceptions and contribute to a positive patient experience?
At Qualtrics, we work with hundreds of healthcare organizations to help them modernize their feedback programs and transform how they operate to put patients and families at the heart of every decision.
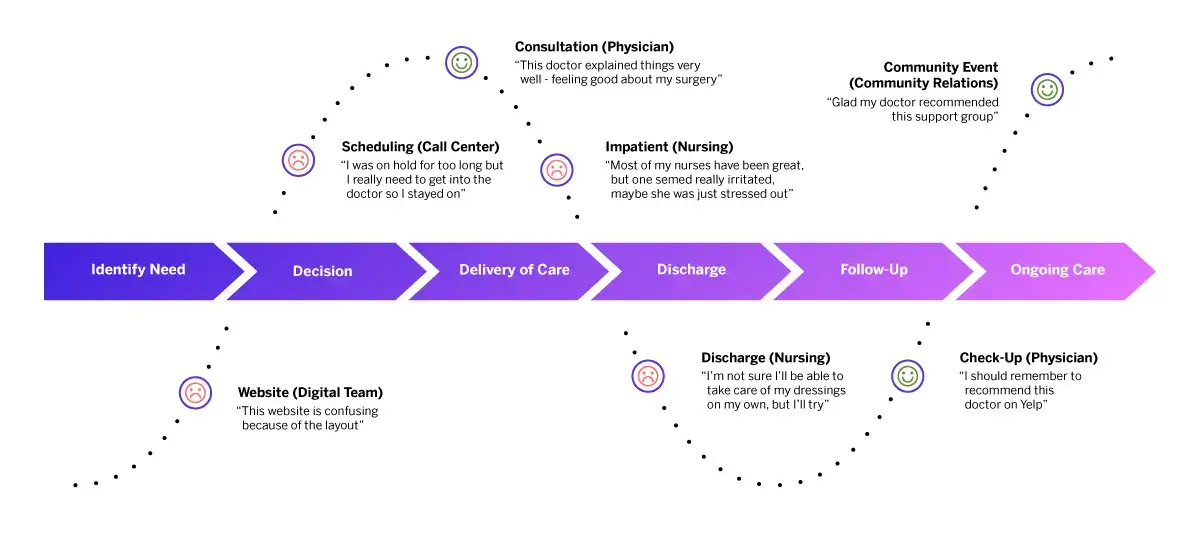
Patient experience feedback can be captured at all stages of the patient journey, from identifying needs to ongoing care.
It comes down to three key things — listen, understand, and act.
We know that a single interaction isn’t the only factor that influences patient experience. And today, patients interact with healthcare across myriad platforms, from social media, apps, and websites to more traditional settings like contact centers, clinics, and hospitals.
In a single journey, they’re most likely to use multiple channels. That can include reading online reviews in their search for a new provider, phoning to make an appointment or to check their coverage, receiving healthcare advice virtually, or visiting a physical location to receive care. Every one of those touchpoints come together to impact the overall patient experience, and not meeting their expectations on any one of those channels can make a difference.
Collecting patient feedback
There are a million ways to gather feedback on various parts of the patient experience, and the information you garner will depend on the methods used.
All patient feedback – regardless of your capture method or type – will explore five facets of the overall patient experience:
- Experiences: What actually happens to a person during an interaction.
- Expectations: What a person anticipates will happen during an experience. This can be heavily influenced by previous interactions.
- Perceptions: How a person views an experience based on their expectations, which are viewed across three dimensions: Success (can they achieve their goals), Effort (how easy or hard is it), and Emotion (how does it make them feel).
- Attitudes: How someone feels about the organization or provider.
- Behaviors: How a person chooses to interact with an organization or provider, which is heavily influenced by that person’s attitudes.
Collecting this patient experience information can be done in many different ways, but two important informational sources drive successful listening strategies:
Patient experience programs
The challenge for many healthcare providers is that traditionally, each channel has existed in a silo. Modern patient experience programs break down those silos by installing listening posts across all channels and bringing the data together into a single system.
This enables you to understand – across the entire patient journey – how each process contributes to the patient experience, and identify actions across the organization that you can take to improve it.
Patient experience surveys
Surveys may seem old hat in a world where omnichannel analytics can capture patient experience data from millions of sources. But they’re tried and tested, and often the best way for patients to tell you how they’re really feeling.
The key here is what you do with patient survey data. While responses have traditionally been viewed in isolation, the trick is to feed survey data into patient experience programs that can make this one informational source part of a larger whole.
How to measure patient experience
Taking patient experience from a set of abstract values and feelings to something that can be objectively measured requires metrics and Key Performance Indicators (KPIs).
Which KPIs a healthcare provider or organization wants to track will depend on their short and long-term goals, but here are some of the most relevant when it comes to measuring patient-centered care:
| Clinical experience | Service quality metrics | Patient engagement | Loyalty and advocacy | Safety and trust metrics |
|---|---|---|---|---|
| Wait times (appointment, waiting room duration) | Cleanliness and comfort of healthcare facilities | Patient portal usage and satisfaction | Net Promoter Score (NPS) | Care providers' perceived safety |
| Provider communication ratings | Staff courtesy and professionalism | Follow-up appointment adherence | Patient retention rates | Trust in medical decisions |
| Care coordination (handoffs between departments and care providers) | Ease of scheduling appointments | Medication adherence rates | Likelihood to recommend to others | Privacy protection confidence |
| Satisfaction with health outcomes | Clarity of billing and insurance processes | Understanding of discharge instructions | Social media sentiment and online reviews | Medication error experiences |
| Healthcare quality | Likelihood to follow care recommendations | Clarity of safety protocols |
Understand your patients and tailor the experience
Having all your patient feedback in one place is a great starting point, but you need to be able to mine that patient experience data for rich insights.
Whether it’s structured data from your regulatory surveys, unstructured data from open-text feedback like online reviews or chatbot interactions, or operational data from your electronic medical record, you must analyze it as a single data set to make sense of it all.
This means you’re not only breaking down silos to get a complete view of the patient experience, you’re also able to understand how each touchpoint is affecting it. This also allows you to personalize the patient experience by understanding what each person’s expectations and motivations are – so you can tailor the experiences you deliver at every touchpoint to ensure you meet their needs.
Improve patient experience: Act on insights at every level

In many organizations, this is where a lot of feedback programs fall short. Typical patient experience surveys can take you only so far. Insights are often delivered long after an interaction has occurred – when it’s probably too late to act on them – and often to senior leaders rather than the people who can do something about it.
As the industry responded to the challenges of COVID-19, we saw just how vital it is that healthcare organizations are able to take action quickly as patient needs change. A patient experience program needs to provide real-time insights at every level of the organization, alerting individuals to things they can do in the moment to help with quality improvement efforts.
For example, if a patient has an issue with a prescription after a visit to a clinic, that negative experience can be resolved immediately by triggering a call from a contact center agent to the provider who can rectify the situation the same day.
These one-to-one interactions are known as the “inner loop” — individual, real-time follow-up that enables you to step in and improve the patient experience. But there’s also the “outer-loop”, too — the more strategic actions that happen at an organization-wide level to solve the root cause of bad experiences.
Take our prescription issue again. Perhaps it was caused by a processing error that could potentially affect multiple patients. As well as closing the loop to resolve it at an individual level, you can also drive action at an organizational level and prevent it from being a problem for other patients in the future.
Imagine that in a system where reports are received once a year and delivered to a handful of senior executives, the same prescription issue could rear its head time and time again, impacting the experience of more patients, and costing the provider a small fortune in recovery costs.
How a culture of action drives patient experience
Having the systems in place to empower individuals in the organization, at every level, to take action helps drive a cultural change, too – one where everybody understands and has the tools to create a positive patient experience. Your people, whether it’s nurses and doctors at the bedside, clinic administrators managing operations, or contact center agents, need to be able to access insights, and feel empowered to act on them.
But beyond that, they need to share the values and vision of the organization. If they understand the expectations and have the training and resources to deliver on them, then you’re far more likely to deliver a good patient experience.
As such, patient experience and employee experience go hand-in-hand. It’s the same approach with staff as it is with patients — gather feedback at every stage in the employee journey, understand the key drivers of the experience, and take action to improve them. Whether that’s improving manager effectiveness and employee engagement, or identifying opportunities to improve key stages in the employee journey – like onboarding or training – it all comes down to knowing which actions to take, and at what stage, to help your people be more successful.
It’s a key part of experience management, both in healthcare and other industries. At Qualtrics, we understand that no experience exists in a silo — engaged, motivated, and enabled staff are the interface between patients and the healthcare system. When staff have a good experience, patients are more likely to have the same.
Patient experience 2.0: How Qualtrics can help
The healthcare industry has come a long way in the last decade. In the past year alone the pace of change has accelerated as the industry demonstrated that it is willing and able to respond quickly to the needs of patients.
The momentum we’ve built up is the starting point of a new era of healthcare – where every decision is taken with the patient experience in mind.
We have the tools, technology, and the desire to deliver patient-centered healthcare facilities of all shapes and sizes.
Our dedicated healthcare team already works with over 400 health systems around the world to help them design and improve the experiences they deliver for staff and patients, and we’ve seen some incredible success stories of how, with patients at the center, organizations are rethinking and redefining the experiences they deliver.
With Qualtrics, healthcare providers can:
- Meet regulatory needs while leveraging leading innovations from outside industries, pushing the boundaries on traditional patient experience
- Understand the human behind the experience through omnichannel and unsolicited listening – with insight into how your patients feel and what they need in the moment
- Empower caregivers and the frontline with complete situational awareness, enabling them to deliver superior care and re-connect them to their purpose
- Use one seamless, secure, flexible platform to co-innovate and exceed your patient experience expectations
Free eBook: 2025 healthcare experience trends report